Protection against COVID-19: experience is not always an advantage for the immune response
A good response to the SARS-CoV-2 vaccination is based on naive immune cells, whereas pre-existing memory cells are rather disadvantageous, as shown by a research team from the Cluster of Excellence PMI.
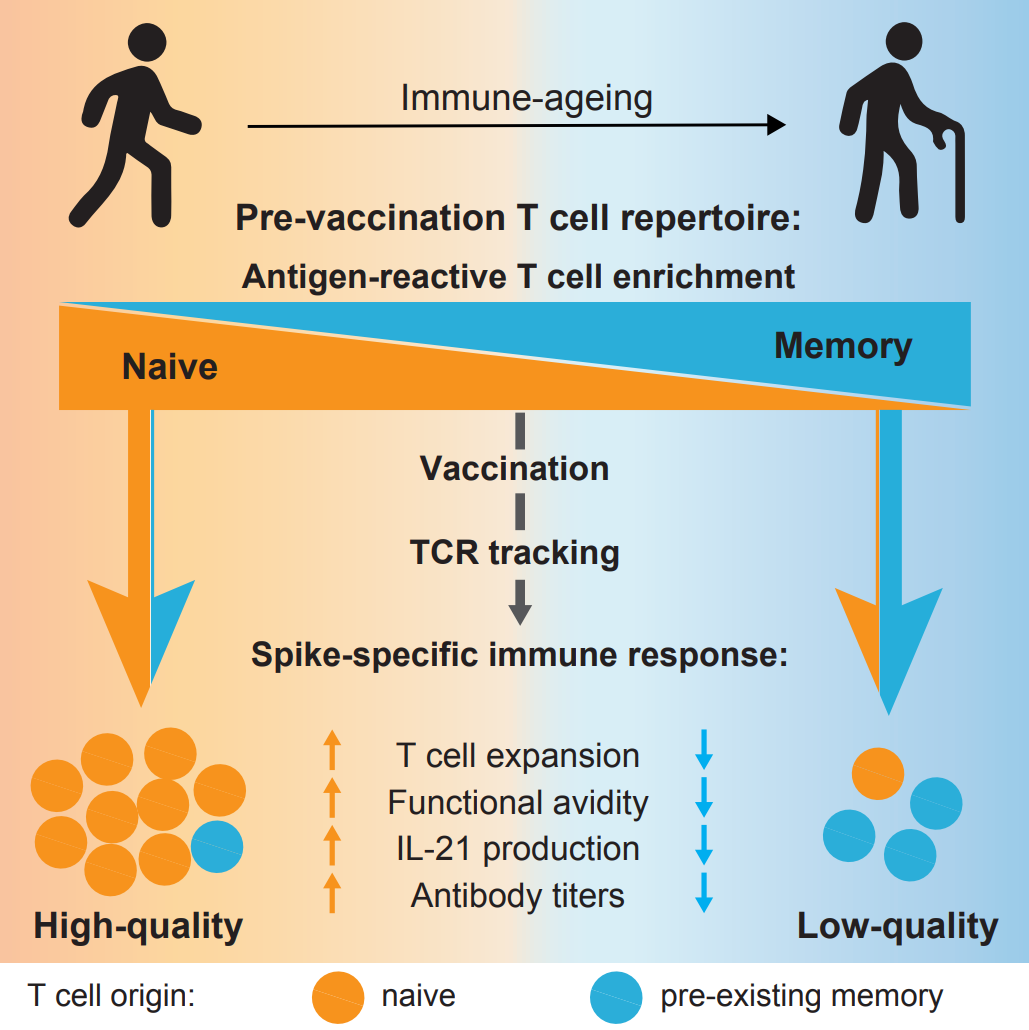
People who have often been infected by common cold viruses – which also belong to the coronaviruses – are not better protected against COVID-19, neither after infection with SARS-CoV-2 nor after vaccination. "We already showed in 2020 that earlier exposure to common cold viruses does not provide protection against COVID-19. In a follow-up study, we have now been able to show that this is also not beneficial for the quality of the vaccine response," explains Professor Petra Bacher from the Institute of Immunology at Kiel University (CAU) and the University Medical Center Schleswig-Holstein (UKSH), Campus Kiel. Together with Professor Alexander Scheffold, Head of the Institute of Immunology, and colleagues from the Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) in Kiel, the immunologist analysed blood samples from healthy people before and after they received the SARS-CoV-2 vaccination. The result of the study has now been published in Immunity: “A good immune response comes from the naïve T cell repertoire. Pre-existing memory T cells that recognise SARS-CoV-2 rather have a negative effect." This could explain why the immune response in the elderly is often worse after infection or vaccination.
What makes a good vaccine response?
T cells, more precisely T helper cells, are the central organisers of immune responses. Each T cell recognises a specific pathogen via its "T cell receptor". Naive T cells have not yet had any contact with a pathogen. During an infection or vaccination, only the pathogen-specific T cells are activated and can transform into memory cells. These memory cells provide a rapid immune reaction upon repeated contact with the pathogen – the principle of vaccination. However, also in the blood of people who are neither vaccinated nor have been infected, memory cells can be found that can react to SARS-CoV-2 but that originate from infections with other pathogens. This is a phenomenon called cross-reactivity, which was previously thought to be protective. “We wondered whether memory cells that have already reacted to a pathogen similar to SARS-CoV-2, such as a cold virus, actually improved the response to the SARS-CoV-2 vaccination. Or whether it is more important to have many naive cells against SARS-CoV-2 that could adapt specifically to the new pathogen. This is typically the case in young people, who usually cope well with infections and vaccinations," explains Professor Bacher, who received the Dorothea Erxleben Female Investigator Award 2021 from the Cluster of Excellence PMI and invested the prize money in this project.
For the current study, the blood of 50 healthy individuals was analysed before they received the corona vaccination and several weeks after the first and second vaccinations. Previous infection with COVID-19 was excluded. Using a special technique called antigen-reactive T-cell enrichment, it is possible to analyse very specifically those cells that react to the vaccine. Bacher: "We sort out the cells that react to SARS-CoV-2 because only they determine the immune response. By analyzing the T cell receptor, an identifier of an individual T cell and its progeny, we can then determine whether the cells came from the naive repertoire or from the memory repertoire." The results of this analysis were correlated to the quality of the vaccine response.
Vaccination success not so good in the elderly
According to Professor Bacher, the result of the study was that "pre-existing memory T cells do not contribute to a high-quality immune response. Rather the opposite. A very good immune response comes from the naive repertoire." Participants over 80 years showed an overall weaker vaccine response. In their cases, the vaccination resulted in only a slight increase of SARS-CoV-2-specific T cells. "We showed that in the eldery, the few naive T cells that remain, can no longer be activated as well. But also the strong presence of pre-existing memory cells does not contribute positively to the vaccine response in the elderly." This defect in older people's immune systems can be alleviated with further booster vaccinations, but it cannot be fully compensated. Despite vaccination, the very old people remain a vulnerable group. “We need to be aware that there is still a group that is at risk. This affects mainly the elderly, whose immune systems cannot cope well with this 'new' pathogen. But also among young people there are some with poor vaccination response. This is also evident from the fact that, despite being vaccinated, serious cases are still occurring," adds Alexander Scheffold.
Vaccination protection – antibody values alone are not conclusive
How well and how long the vaccination protects against SARS-CoV-2 in individual cases can still not be reliably determined by blood tests. The measurement of specific antibodies against the pathogen is not conclusive because we do not know yet at what level sufficient immune protection is given. Bacher said: "There are no clear thresholds in the immune system. Which factor is decisive can vary from person to person. Overall, many parameters contribute to protection against infection, in addition to antibodies, in particular the T cells." However, the T cell analyses used in this study are still far too complex for clinical application. There is still a lot to be invested in research and development before we can determine these organisers of the immune response in everyday clinical practice, and not just for SARS-CoV-2. However, the COVID-19 pandemic has clearly demonstrated the need for this.
Original Publication
Carina Saggau, Gabriela Rios Martini, Elisa Rosati, …, Alexander Scheffold, Petra Bacher. The pre-exposure SARS-CoV-2 specific T cell repertoire determines immune response quality to vaccination. Immunity (2022)
Doi: https://doi.org/10.1016/j.immuni.2022.08.003
More Information:
- COVID-19: COVID-19: contact with cold viruses apparently offers no protection (press information Nov. 30th, 2020)
Contacts
Prof. Petra Bacher
Institute of Immunology and Institute of Clinical Molecular Biology, CAU and UKSH
+49 431 500-31005
Petra.Bacher@uksh.de
Prof. Alexander Scheffold
Institute of Immunology, CAU and UKSH
+49 431 500-31000
Alexander.Scheffold@uksh.de
Prof. Petra Bacher, member of the Cluster of Excellence PMI and Schleswig-Holstein Excellence-Chair early career group leader at the Institute of Immunology and Institute of Clinical Molecular Biology, CAU and UKSH.
Prof. Alexander Scheffold, member of the PMI Steering Committee, Director of the Institute of Immunology, CAU and UKSH.
About the Cluster of Excellence PMI
The Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) is being funded from 2019 to 2025 through the German Excellence Strategy (ExStra). It succeeds the "Inflammation at Interfaces” Cluster, which was already funded in two periods of the Excellence Initiative (2007-2018). Around 300 members from eight institutions at four locations are involved: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design, Kiel Institute for the World Economy (IfW), Leibniz Institute for Science and Mathematics Education (IPN)), Lübeck (University of Lübeck, University Medical Center Schleswig-Holstein (UKSH)), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel - Leibniz Lung Center).
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to healthcare more intensively, as well as to fulfil previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
Press contact
kerstin.nees@hamburg.de+49 431 880-4682
Cluster of Excellence "Precision Medicine in Chronic Inflammation"
Scientific Office
Head: Dr. habil. Susanne Holstein Postal
Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
+49 (0)431 880-4850, fax: +49 (0)431 880-4894
spetermann@uv.uni-kiel.de
Twitter: PMI @medinflame