How chronic intestinal inflammation can cause cancer
A Kiel research team from the Cluster of Excellence "Precision Medicine in Chronic Inflammation" has found a novel mechanism which can disrupt DNA repair in patients with chronic intestinal inflammation and thus lead to bowel cancer.
Chronic inflammatory bowel disease (IBD) are inflammations of the gastrointestinal tract which flare up in phases and are accompanied by bloody bowel movements, diarrhea and severe impairment of the quality of life. IBD patients exhibit an increased risk of developing colorectal cancer. This is facilitated by the fact that DNA in the intestinal mucosa cells (intestinal epithelium) is damaged by chronic inflammatory processes. Upon DNA damage, a cell in a healthy state protects itself from accumulation of a defective genome by not dividing further. However, these protective mechanisms are suspended under inflammatory conditions, which promotes the development of bowel cancer. It is not yet understood why these protective mechanisms become dysfunctional in the event of chronic inflammation.
A team from the Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) has now shown that the gene XBP1, which is a risk gene for IBD, has a decisive influence on how an intestinal mucosa cell deals with DNA damage, and thus protects itself against the development of cancer. In addition, the team led by Professor Philip Rosenstiel and PD Dr. Konrad Aden from the Institute of Clinical Molecular Biology (IKMB) at Kiel University (CAU) and the University Medical Center Schleswig-Holstein (UKSH), Campus Kiel, was able to find initial indications of the possible underlying mechanism. They published their results in the renowned scientific journal "Gastroenterology".
Risk gene worsens DNA repair
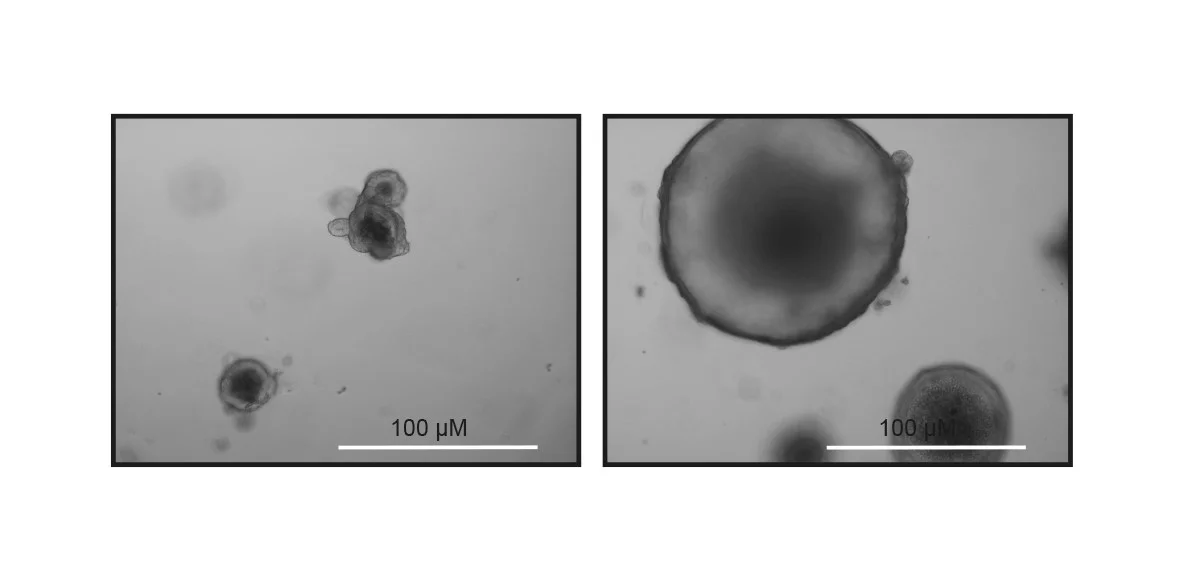
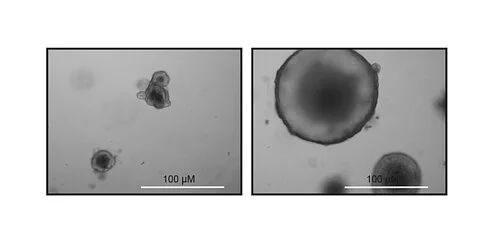
In a healthy, non-altered state, the gene XBP1 encodesa protein that ensures the molecular balance in the intestinal mucosa and protects against inflammation. In IBD patients, a loss of function of this gene in the intestine can lead to a disturbed barrier and unhindered inflammation. In the newly-published study, the Kiel research team has shown that the gene could also play a role in the emergence of bowel cancer. If the gene is missing in the surface cells of the intestinal mucosa, an important repair mechanism of the genetic material is no longer carried out correctly. "If the IBD risk gene XBP1 is missing in intestinal epithelial cells, then DNA damage and increased cell division will occur. Animals with a defective XBP1 gene developed invasive intestinal cancer," reported the first author Lina Welz, who as a clinician scientist at the Cluster of Excellence PMI is conducting doctoral research at the IKMB while completing her specialist medical training in parallel at the Department of Internal Medicine I at the UKSH, Campus Kiel.
Mechanism via tumor suppressor p53 and mTOR signaling pathway
In the next step, the researchers wanted to understand precisely which mechanism the gene XBP1 uses to regulate DNA repair, and which thus leads to cancer in the event of XBP1-malfunction. The researchers discovered an important role of the already-known molecular switch p53, a so-called tumor suppressor, which protects the cell from malignant degeneration. p53 is considered a "guardian of the genome" and plays a decisive role in controlling cell growth. The research team was able to show that XBP1 coordinates the activity of the p53 tumor suppressor. They also managed to identify a new mechanism through which the tumor suppressor p53 prohibits uncontrolled growth of intestinal epithelial cells. "Our results indicate that XBP1 and p53 work together via the so-called mTOR signaling pathway to prevent a damaged intestinal epithelial cell undergoing uncontrolled proliferation, and thus becoming malignant," said one of the senior authors PD Dr. Konrad Aden, senior clinician scientist at the Cluster of Excellence PMI and senior physician at the Department of Internal Medicine I at the UKSH, Campus Kiel.
Potential therapeutic approach
In medicine, the mTOR signaling pathway has long been used as a therapeutic target for other diseases, and could provide a new early access for cancer treatment. The researchers treated mice and cell systems that display increased DNA damage and a defective XBP1 gene with a specific inhibitor of the mTOR pathway, the pharmacological substance Rapamycin. “In our models, Rapamycin significantly reduced the increased cell division and the resulting damage to the intestinal epithelium," reported Aden.
"Although we have known for a long time that cancer can arise from chronic intestinal inflammation, we only know relatively little about the underlying processes. Our results now provide a new link between inflammation, disturbed cell division and repair of genetic material," reported senior author Professor Philip Rosenstiel, director of the IKMB. "We will therefore in further studies investigate how targeted inhibition of the mTOR signaling pathway can be used to prevent intestinal inflammation and cancer," said Rosenstiel.
"This scientific success of a clinician scientist at the cluster also proves the effectiveness of the clinician scientist program in the Cluster of Excellence PMI, which enables physicians to conduct research on an equal basis at the same time as their specialist medical training. The freedom to research created in this way and the good scientific infrastructure enables clinically active doctors, such as Lina Welz, to achieve such outstanding scientific achievements," emphasized Professor Stefan Schreiber, PMI spokesperson, director of the IKMB, CAU and UKSH, and director of the Department of Internal Medicine I at the UKSH, Campus Kiel.
Original publication:
Welz L, Kakavand N, Hang X, Laue G, Ito G, Silva MG, Plattner C, Mishra N, Tengen F, Ogris F, Jesinghaus M, Wottawa F, Arnold P, Kaikkonen L, Stengel S, Tran F, Das S, Kaser A, Trajanoski Z, Blumberg R, Roecken C, Saur D, Tschurtschenthaler M, Schreiber S, Rosenstiel P and Aden K. Epithelial XBP1 coordinates TP 53-driven DNA damage responses and suppression of intestinal carcinogenesis. Gastroenterology (2021), https://doi.org/10.1053/j.gastro.2021.09.057
Scientific Contact:
Lina Welz
Department of Internal Medicine I, UKSH Kiel
Institute of Clinical Molecular Biology, CAU, UKSH
0431/500-62011
l.welz@ikmb.uni-kiel.de
PD Dr. Konrad Aden
Department of Internal Medicine I, UKSH
Institute of Clinical Molecular Biology, CAU, UKSH
0431/500-15167
k.aden@ikmb.uni-kiel.de
Prof. Dr. Philip Rosenstiel,
Institute of Clinical Molecular Biology, CAU, UKSH
0431/500-15111
p.rosenstiel@mucosa.de
About the Cluster of Excellence PMI
The Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) is being funded from 2019 to 2025 through the German Excellence Strategy (ExStra). It succeeds the "Inflammation at Interfaces” Cluster, which was already funded in two periods of the Excellence Initiative (2007-2018). Around 300 members from eight institutions at four locations are involved: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design, Kiel Institute for the World Economy (IfW), Leibniz Institute for Science and Mathematics Education (IPN)), Lübeck (University of Lübeck, University Medical Center Schleswig-Holstein (UKSH)), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel - Leibniz Lung Center).
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to healthcare more intensively, as well as to fulfil previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
Press office
fbuhse@uv.uni-kiel.de+49 (0)431/880 4682 https://precisionmedicine.de
Cluster of Excellence "Precision Medicine in Chronic Inflammation"
Scientific Office
Head: Dr. habil. Susanne Holstein Postal
Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
+49 (0)431 880-4850, fax: +49 (0)431 880-4894
spetermann@uv.uni-kiel.de
Twitter: PMI @medinflame