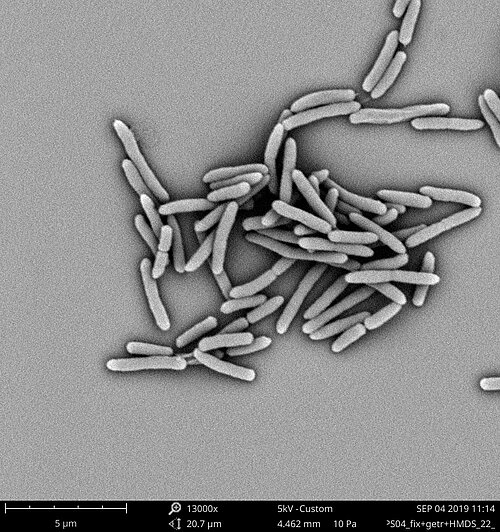
Undetected and difficult to treat: multidrug resistant tuberculosis strain
Research team finds multidrug resistant TB-strain in Eswatini, that is not detected by modern diagnostic methods and has developed resistance to the new antibiotic bedaquiline.
More than a third of multidrug-resistant (MDR) tuberculosis (TB) cases in Eswatini, in Southern Africa, are caused by an outbreak strain that cannot be correctly detected by currently used molecular biological tests such as Xpert MTB/RIF. In addition, in 50% of the cases, this strain has also acquired mutations that confer resistance to two important drugs for treatment of MDR-TB, a novel drug, bedaquiline and a repurposed drug, clofazimine. The results of this work have now been published by the research team around Professor Stefan Niemann from the Research Center Borstel Leibniz Lung Center and the German Center for Infection Research (DZIF) in the journal Genome Medicine.
Rapid molecular detection of MDR-TB cases is key to the effective treatment of MDR-TB patients and control of the drug resistance TB transmission. In Eswatini, the WHO recommended Xpert MTB/RIF test is used nationwide as a front line MDR-TB diagnostic test to guide prompt MDR-TB treatment according to the latest WHO guidelines. Both, bedaquiline and clofazimine, are important components for the treatment of MDR-TB patients.
In this study that has been conducted under the leadership of scientists at the Research Center Borstel and the German Center for Infection Research with collaboration from different institutions, a total of 144 MDR-TB isolates collected in Eswatini over two periods (2009-2010, 2014-2017) were analyzed using whole genome sequencing. This analysis showed that more than 30% of the MDR TB isolates belong to one outbreak strain, which has a specific rifampicin resistance mutation not detected by the Xpert MTB/RIF rapid test and other molecular methods for resistance detection. Recent data from an independent study show that the outbreak strain with this specific mutation now accounts for more than 50% of MDR-TB isolates in Eswatini.
In addition, 50% of the patient isolates of the outbreak strain also had mutations conferring resistance to the important MDR-TB treatment drugs bedaquiline and clofazimine. This finding was particularly astonishing, since bedaquiline and clofazimine have only been used in recent years for the therapy of MDR-TB patients. Together with a very high resistance rate to classical TB drugs, the treatment of MDR-TB patients infected with the outbreak strain is thus very difficult and requires a comprehensive resistance diagnosis and tailored drug therapy.
"The high proportion of this outbreak strain in the country is a major problem for the control of the MDR-TB epidemic in Eswatini", says senior author Prof. Niemann, who also holds a Schleswig-Holstein Excellence Chair, is a member of the executive group of the Cluster of Excellence “Precision Medicine in Chronic Inflammation” (PMI) and spokesperson of the Leibniz Science Campus EvoLUNG. "There is a considerable risk for the outbreak strain to spread further and seriously complicate treatment of the afflicted patients will due to its inherent resistance to most drugs used in tuberculosis therapy”.
This study also raises fundamental points regarding the development and introduction of novel anti-TB agents. Indeed, the assumption that all isolates are equally susceptible to a new agent does not apply in all settings and can be influenced by the presence of particular strain types. It also questions the role of rapid molecular tests such as Xpert MTB/RIF in regions with high prevalence of such isolates and underlines the importance of methods such as genome sequencing that can detect all cases of MDR-TB.
Scientists from the Research Center Borstel are therefore working closely with the local authorities in the SeqMDRTB_NET consortium a project in the framework of the Global Health Protection Programme funded by the German Federal Ministry of Health to establish new diagnostic procedures based on the genetic analysis of tuberculosis strains in Eswatini and thereby strengthen the diagnostic capacities in the country.
"In addition, further analysis of the ongoing spread of the outbreak strain in Eswatini and neighboring countries is needed to adapt tuberculosis control measures where necessary," says Patrick Beckert, one of the study's lead authors.
Scientific contact:
Prof. Dr. Stefan Niemann
Research Center Borstel
+49 4537 188 7620
sniemann@fz-borstel.de
Prof. Stefan Niemann, Borstel Research Center and German Center for Infection Research, Schleswig-Holstein Excellence Chair at the University of Lübeck, Member of the Group of the Cluster of Excellence PMI and Spokesperson of the Leibniz Science Campus EvoLUNG.
Original publication:
P. Beckert*, E. Sanchez-Padilla*, M. Merker* et al.: MDR M. tuberculosis outbreak clone in Eswatini missed by Xpert has elevated bedaquiline resistance dated to the pre-treatment era. Genome Med 12, 104 (2020). https://doi.org/10.1186/s13073-020-00793-8
*These authors contributed equally to the work
About the Cluster of Excellence PMI
The Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) is being funded from 2019 to 2025 through the German Excellence Strategy (ExStra). It succeeds the "Inflammation at Interfaces” Cluster, which was already funded in two periods of the Excellence Initiative (2007-2018). Around 300 members from eight institutions at four locations are involved: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design, Kiel Institute for the World Economy (IfW), Leibniz Institute for Science and Mathematics Education (IPN)), Lübeck (University of Lübeck, University Medical Center Schleswig-Holstein (UKSH)), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel - Leibniz Lung Center).
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to healthcare more intensively, as well as to fulfil previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
Press office
fbuhse@uv.uni-kiel.de+49 (0)431/880 4682 https://precisionmedicine.de
Cluster of Excellence "Precision Medicine in Chronic Inflammation"
Scientific Office
Head: Dr. habil. Susanne Holstein Postal
Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
+49 (0)431 880-4850, fax: +49 (0)431 880-4894
spetermann@uv.uni-kiel.de
Twitter: PMI @medinflame