Aging brain: part of the innate immune system regulates the blood-brain barrier
German-American research team demonstrates the role of the complement system in the aging process of the brain.
As a person becomes older, many structures and functions in the brain change. An important age-related change is the increased permeability of the blood-brain barrier, which normally only allows certain substances from the bloodstream into and out of the brain. Among other things, this may favor the development of neurodegenerative diseases such as Alzheimer's dementia. A series of previous studies suggests that the reduced function of the blood-brain barrier is linked to immunologically-related inflammatory processes – however, the exact mechanisms behind this are still hardly understood. In laboratory tests, Professor Jörg Köhl, board member of the Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) and director of the Kiel Institute for Systemic Inflammation Research (ISEF), University of Lübeck (UzL) and University Medical Center Schleswig-Holstein (UKSH), Campus Lübeck, together with the working group led by Professor Hui Zheng (Huffington Center on Aging, Houston, USA), have now identified a mechanism by which the so-called complement system, a specific part of the immune system, regulates the vascular inflammation and associated disturbed function of the blood-brain barrier during the aging process. The researchers recently published their findings in the renowned scientific journal "Journal of Clinical Investigation”.
The complement system is part of the innate immune system. It consists of more than 40 proteins, which are present in the blood and as receptors on the surface of cells. These proteins include the so-called complement factors and their cleavage products (protein fragments), as well as receptors that recognize these fragments. The system plays an important role in the defense against microorganisms. It signals the presence of pathogens as well as the binding of antibodies to pathogens, but also to the body's own structures. However, faulty regulation of the complement system may result in an excessive inflammatory response in the course of certain diseases, which causes tissue damage. While most of the complement proteins are produced in the liver, it has long been known that both complement factors as well as complement receptors are also independently produced directly in the brain. Of particular importance is the complement factor C3, which can be fragmented into two parts, C3b and C3a. C3a triggers its biological effect by binding with the C3a receptor, which is present on cells such as the vascular endothelial cells, i.e. the cells which form the inner lining of blood vessels, as well as various brain cells.
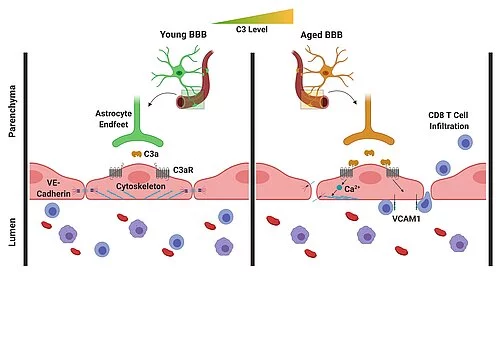
In the recently-published study, the researchers were able to show that C3/C3a production increases in the aging brain, and there is activation of the C3a receptor on vascular endothelial cells of the brain. In response, these cells increasingly produce a certain adhesion molecule, leading to an increased migration of lymphocytes (special immune cells) into the brain. In addition, the activation of the C3a receptor on the vascular endothelial cells induces the release of intracellular calcium ions. This leads to a disruption of a specific protein on the vascular endothelial cells, which is of primary importance for the binding of these cells. Breaking these bonds causes increased permeability of the blood-brain barrier. This means that the brain is no longer so well separated from the rest of the body, so that inflammations can also spread more easily from the environment to the brain.
In order to investigate this disease mechanism, the researchers developed a transgenic mouse model, in which the mice were genetically altered so that they no longer produce C3a receptors on the vascular endothelial cells. The specific elimination of the C3a receptor in vascular endothelial cells not only protected the mice against an increased permeability of the blood-brain barrier in old age, it also reduced the inflammatory activity of special immune cells in the brain, the microglia cells, and increased the volume of the hippocampus and cerebral cortex of aging mice, in comparison with mice with the C3a receptor. The hippocampus is of particular importance for learning and memory processes.
"Our findings show a new regulatory mechanism of the blood-brain barrier which is controlled by the complement system, and the associated immune cell activation, inflammation and degeneration in the aging brain," said Köhl. "The data suggests that the targeted blocking of individual elements of the complement system could lead to a significant improvement in the vascular function and reduce the permeability of the blood-brain barrier, and thereby a reduction in neuroinflammation and neurodegeneration in old age," added Köhl.
The observations could also be interesting for acute inflammatory conditions such as strokes and traumatic brain injuries or neurodegenerative diseases, in particular Alzheimer's, for which age is the biggest risk factor. "It is known from previous studies that the complement system is also highly activated in these diseases," explained Köhl. "Thus, our findings could in future also enable new therapeutic approaches for these age-related diseases of the brain."
Scientific contact:
Prof. Jörg Köhl
nstitute for Systemic Inflammation Research,
University of Lübeck and University Medical Center Schleswig-Holstein (UKSH), Campus Kiel
+49-451-500-51400
Joerg.Koehl@uksh.de
Professor Jörg Köhl, steering committee member of the Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) and Director of the Institute of Systemic Inflammation Research (ISEF), University of Lübeck (UzL) and University Medical Center Schleswig-Holstein (UKSH), Campus Lübeck.
In the aging brain, C3/C3a production increases and the C3a receptors on vascular endothelial cells of the brain are activated. In response, these cells produce increased amounts of the adhesion molecule VCAM-1, which leads to an increased migration of lymphocytes into the brain. In addition, the activation of the C3a receptor leads to a mobilization of calcium ions in the cells, resulting in a disruption of the vascular endothelial cadherin, which is of central importance for the interconnection of these cells. Breaking these connections results in an increased permeability of the blood-brain barrier.
Original publication:
Propson N.E., Roy E.R. Litvinchuk A., Köhl J., Zheng H.: Endothelial C3a receptor mediates vascular inflammation and BBB permeability during aging.J.Clin. Invest. (2020); first published Sep 29, 2020. DOI: 10.1172/JCI140966
About the Cluster of Excellence PMI
The Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) is being funded from 2019 to 2025 through the German Excellence Strategy (ExStra). It succeeds the "Inflammation at Interfaces” Cluster, which was already funded in two periods of the Excellence Initiative (2007-2018). Around 300 members from eight institutions at four locations are involved: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design, Kiel Institute for the World Economy (IfW), Leibniz Institute for Science and Mathematics Education (IPN)), Lübeck (University of Lübeck, University Medical Center Schleswig-Holstein (UKSH)), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel - Leibniz Lung Center).
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to healthcare more intensively, as well as to fulfil previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
Press office
fbuhse@uv.uni-kiel.de+49 (0)431/880 4682 https://precisionmedicine.de
Cluster of Excellence "Precision Medicine in Chronic Inflammation"
Scientific Office
Head: Dr. habil. Susanne Holstein Postal
Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
+49 (0)431 880-4850, fax: +49 (0)431 880-4894
spetermann@uv.uni-kiel.de
Twitter: PMI @medinflame